Osteochondrosis of the second degree of the cervical spine requires professional treatment. With the development of this pathology, the integrity of the intervertebral discs is disturbed, and the gap between them also decreases. Of all the forms of osteochondrosis, cervical is the most common. The neck is mobile, in this sense, it is regularly subjected to stress. The initial stage of osteochondrosis is normally tolerated. Released - Poses a great threat to health.
Why does osteochondrosis of the cervical spine occur?
The causes of cervical osteochondrosis are numerous. The pathology can develop in people who lead a sedentary lifestyle. The veins pass through the vertebrae in the cervical region and supply blood to the vessels of the brain. SHOP osteochondrosis often occurs due to increased stress on the neck. Spinal osteochondrosis of the first degree occurs in young and old people. It is not the age that plays an important role, but the lifestyle and the characteristics of the body.
Second-degree cervical osteochondrosis is common among adolescents. In medicine, there is the concept of "adolescent osteochondrosis". A common cause of 1. 2 degree osteochondrosis is the wrong position of the head. When this disease develops, the pulp breaks. The types of osteochondrosis depend on how pronounced the pulp rupture is. Untimely treatment of osteochondrosis of the first degree leads to the progression of the pathological process. In the third stage of the disease, degenerative-dystrophic processes are pronounced: the patient is more concerned with pain in the back and neck.
Characteristics of the first stage
With osteochondrosis of the cervical spine of the first degree, the pathological process spreads to the muscles. The initial stage is characterized by the formation of cracks in the fibrous ring. It is made up of collagen fibers.
Osteochondrosis of the first degree of the cervical spine leads to the appearance of uncomfortable symptoms:
- The first stage of osteochondrosis is manifested by pain in the back of the head. Some people swell. With cervical osteochondrosis of the first degree, severe cramping pains may appear.
- If a person has been diagnosed with osteochondrosis of the cervical spine, he should visit an ophthalmologist. The pupils can be dilated.
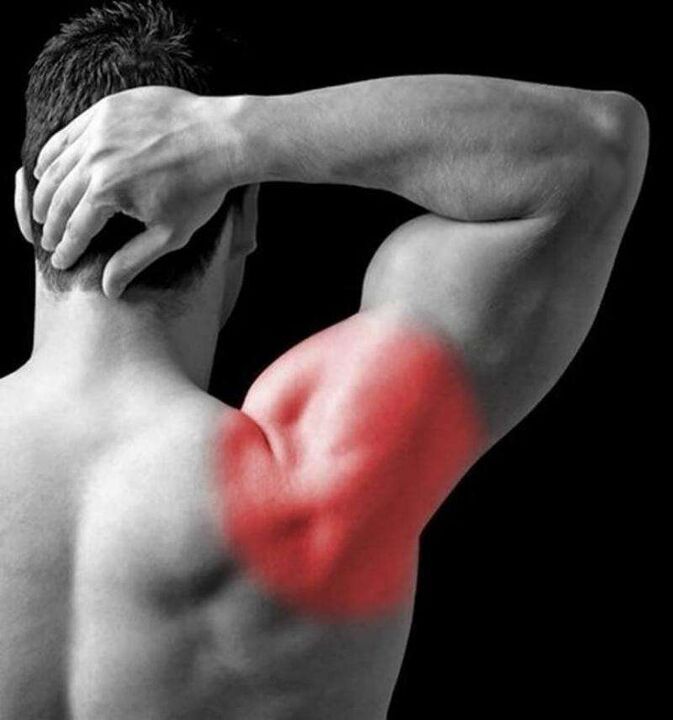
- First-degree cervical osteochondrosis often leads to Wright's syndrome. If the patient puts his hand behind his head, the pain intensifies.
- Cervicalgia syndrome usually develops early in the disease. Inflammation in this case affects the muscles. The progression of cervicalgia syndrome is associated with an abscess. A person begins to feel pain in the neck, the mobility of the joints is limited.
- In the first stage, an anterior scalene muscle syndrome may appear, in the event that the subclavian artery is affected.
How is the treatment carried out? The goal of therapy is to repair pulp tears and prevent unpleasant symptoms. Treatment of osteochondrosis of the cervical spine is carried out surgically. The postoperative duration is 7 days. In a month or two, the sutures gradually come together.
To ensure the prevention of disease, you need to wear a special collar, it is worn around the neck. The doctor recommends using a calcium gluconate solution. The remedy helps to heal wounds.
What happens in the second stage of the disease?
Osteochondrosis of the cervical spine of the second degree develops with the ineffectiveness of therapy at an early stage. Inflammatory reactions become pronounced, the intervertebral foramen decreases.
Grade 2 cervical osteochondrosis leads to the formation of osteophytes. These are bone processes that form in the context of dehydration.
Stage 2 cervical osteochondrosis can last 4 to 5 years. The disease periodically subsides and worsens. A characteristic feature of the disease is head drop syndrome.
Treatment involves manual therapy. The goal is to provide the cervical muscles with normal fixation. Depending on the situation, an orthopedic treatment (connection of the vertebrae) may be prescribed. Drug therapy is required. Calcium chloride is prescribed to eliminate pain. Recovery gymnastics is recommended: should be given 30 minutes a day. The main load should be on the joints.
How does the third stage manifest itself?

Treatment of third-degree osteochondrosis is quite difficult. With this disease, the structure of the intervertebral discs changes.
The pathological process involves tissues and joints:
- The vertebral body is torn, there are characteristic signs of an intervertebral hernia. The person begins to feel severe pain in the back, neck, and extremities. Degenerative-dystrophic reactions affect a large part of the neck.
- Osteochondrosis of the third degree of the cervical spine is characterized by vestibular disorders. Periodically, a person experiences pain in the temples. Some patients may partially lose consciousness.
- The danger of the disease in the third stage is that it leads to endocrine pathology. Therapy involves the operation and the use of manual techniques. In the third stage of cervical osteochondrosis, drugs are not prescribed.
- The patient may have polysegmental osteochondrosis. With this disease, the cervical spine segments are affected, shoulder mobility is impaired, and pain in the elbows appears.

To restore the function of the spine, you must wear a collar.
Disease syndromes
Cervical osteochondrosis is accompanied by syndromes:
- Vertebral occurs when cartilage and bone tissue are involved in the pathological process. Neck mobility is affected. If a person tries to turn his head to the side, pain appears in the occipital region of the neck. The vertebrae undergo morphological changes that are visible on radiography. Symptoms of a syndrome are interrelated. An important sign of vertebral syndrome is morphological changes in cartilage tissues and bone structures. This syndrome is difficult to diagnose. A similar symptom complex is present with myositis.
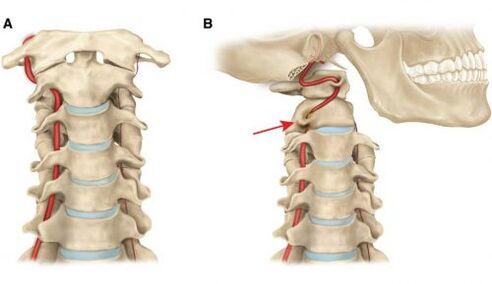
- Vertebral artery syndrome is another manifestation, it can occur regardless of the degree of cervical osteochondrosis. The disease process affects the arteries that feed the brain. Periodically, there is a sense of wonder. Vertigo is a symptom of vertebral artery syndrome. Blood pressure can jump, periodically there is nausea, vomiting. The nerve endings are irritated, causing a headache. With vertebral artery syndrome, you may pass out, lack of oxygen. The disease is accompanied by the deposition of atherosclerotic plaques on the walls of blood vessels.
- Cardiac syndrome manifests itself by pain in the sternum. Rapid fatigue and decreased performance are observed. The heartbeat accelerates. Diagnosis includes angiography and functional tests. Root syndrome is associated with damage to the spinal nerves. It is one-sided. With radicular syndrome, neck pain is observed, combined with paralysis.
It should be noted that osteochondrosis damages a large number of vertebrae.
What is osteochondrosis of the thoracic region?
Osteochondrosis of the thoracic spine is detected in young and old people - age does not matter. The pathology leads to degenerative-dystrophic changes in cartilage and bone structures. Late treatment involves a violation of the structure of the intervertebral ligaments, joints and discs. At an advanced stage, thoracic osteochondrosis leads to the destruction of the intervertebral discs.
Complications of the disease can be:
- pneumosclerosis;
- sterility;
- malignant formations.
If the disease develops in a young person, premature aging of the musculoskeletal system is observed. The functioning of cartilage structures and tissues is significantly affected.
Clinical presentation and causes
- With the development of this pathology, chest pains appear. They occur in a quiet position and while driving. Unpleasant sensations intensify after lifting weights, sharp turns.
- The ailment manifests itself by squeezing the back. Respiration is affected as a result of this problem.
- Chills may occur.
- Some people complain of peeling skin, thinning of the nail plate.
The disease is associated with pathological reactions in the intervertebral discs. It can be inherited. A predisposing factor is the defeat of the intervertebral discs. In some people, the disease is diagnosed in the context of osteophytes. The reason may be underdosed physical activity or, conversely, physical inactivity.
Therapeutic activities
If there are no neurological symptoms, complex treatment is still required. Therapy cannot be postponed, otherwise the destruction of the intervertebral discs will occur.

Before starting treatment, a diagnosis is necessary. If a person has identified at least one of the above symptoms, they need to see a neurologist. The doctor will take an anamnesis, explore the thoracic region. Palpation reveals herniated discs. If the doctor finds any, he prescribes an additional examination. Requires radiography. The MRI procedure allows you to study the musculoskeletal system and identify neoplasms.
Treatment depends on the degree of osteochondrosis of the breast; It begins after the diagnosis is confirmed. The doctor prescribes drugs that help relieve pain and restore the functioning of the musculoskeletal system. For the treatment of this pathology, injections, physical therapy, physical therapy exercises are needed. Additional procedures: magnetotherapy, vacuum therapy, physical therapy exercises.
Daily exercise has a complex effect on the body, improves the functioning of the musculoskeletal system and the respiratory system. Massage reduces the severity of pain, increases muscle tone, relieves fatigue, and improves blood circulation in the tissues. The procedure is performed by an experienced specialist.
conclusion
How many years can you live with osteochondrosis of the cervical and thoracic spine? The pathology is not life-threatening, but its symptoms cause serious discomfort. The clinical picture of the disease can change - it all depends on the effectiveness of therapy.














































